"We need to be as accessible to people as possible," said Dr. Postolovska, who
provides women with essential sexual and reproductive health care amid war and constant stress.
Dr. Postolovska, who comes from a family of doctors, decided to devote her life to helping others when she was a schoolgirl. She was so convinced of her choice that at the age of 15, she started working as a nurse in a pharmacy to gain the experience required to enter her dream medical university where she specialized in obstetrics and gynaecology.
“It gives every family a chance to give birth to a healthy child at the expected time," she said. Dr. Postolovska is now the head of the regional centre for family planning, human reproduction, and medical genetic counselling where she has been working for 24 years.

Help on the ground
Dr. Postolovska joined a mobile reproductive health team in May. A total of 3 mobile teams were launched in April by the United Nations Population Fund (UNFPA) as part of the response to the humanitarian crisis in Ukraine. The teams help temporarily displaced women from the regions where active hostilities continue. The teams are equipped with medicines, tools, contraceptives, and tests for HIV, hepatitis, and sexually transmitted diseases.
"Vinnytsia is a transit region,” said Dr. Postolovska. “About 185,000 internally displaced people have passed through since the beginning of the war and 113,000 of those are women. Some of them travelled further, but many have stayed in Vinnytsia."
During five months, Dr. Postolovska, together with a midwife and a therapist, examined about 3,000 patients in six districts of the region - Lypovets, Koziatyn, Lityn, Bar, Nemyriv, and Kalynivka. The visits are planned in coordination with the Health Department and primary health care providers on the ground.
"Community family doctors decide which rural health posts we need to visit,” said Dr. Postolovska. “In particular, it depends on the number of women of reproductive age and IDPs. We don't visit the district centres, but we go to remote villages where there hasn’t been a visit from an obstetrician-gynaecologist for many years. That's why we ended up seeing some clients who had not been examined for fifteen years."
According to Dr. Postolovska, word of mouth works well in such communities. So, there is always a queue of patients waiting for the doctors when they arrive.
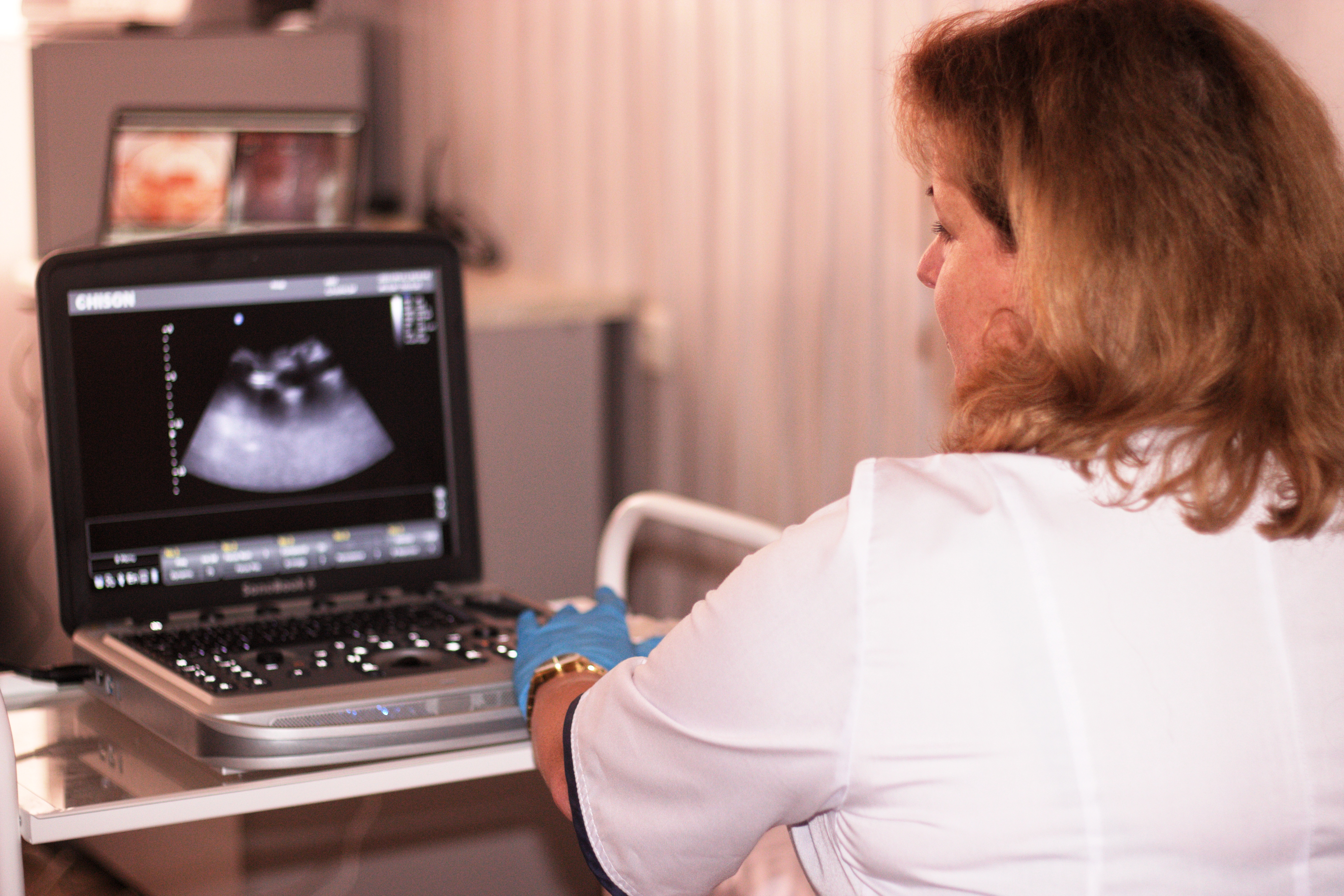
"One day, we examined 43 people in a day in Lityn,” said Dr. Postolovska. “It was difficult because we always conduct a general clinical, gynaecological examination, take a cytological smear, do colposcopy, ultrasound, as well as a breast examination. It's not easy, but we can't stop the arrival of patients just because we feel tired. We need to examine everyone."

Two-thirds of women have pathologies
“More than two-thirds of the examined patients had some kind of pelvic disease,” said Dr. Postolovska. “The most common gynaecological problems are menstrual irregularities, premenstrual syndrome, benign uterine tumours, and dysplasia. Menstrual disorders are a consequence of stress. Also, the number of miscarriages have increased by 10-15 per cent compared to the pre-war period. After an initial examination, we refer such clients to our centre in Vinnytsia for further treatment with geneticists.”
In addition to a gynaecologist, the mobile reproductive health team also has a therapist. This means men can also receive essential assistance. The most common problems for men are cardiac diseases, which, according to Dr. Postolovska, make up about 60 per cent of the total number of male patients. Diseases of the endocrine system, in particular, diabetes, problems with the gastrointestinal tract, musculoskeletal system, respiratory system, and ENT organs are also widespread in men.
Lack of a self-care culture
According to Dr. Postolovska, the main challenges for the team - when assisting people from remote communities - are a historic lack of medical assistance and an absence of self-care when it comes to health.
"In one village we met a woman in her tenth year of menopause with an intrauterine device, which she had installed 30 years ago, but they should only be used for three years. And that is not the worst case. We have also detected large fibroids, erosion, and dysplasia, which women live with for decades without even realizing the danger."
People of all ages, including teenagers, visit the mobile teams for consultations. However, the average age of patients is between 37 and 42 years old.
"We have also visited remote communities where all the patients are over 65 years old,” she said. “However, closer to Vinnytsia, there are more women of reproductive age. The population has also become younger because of the number of displaced women who have arrived."

Working with IDPs, doctors require psychological support
Working with internally displaced people can be stressful for doctors.
"During our visit, we try to see internally displaced women first because they are the primary focus of our mission,” said Dr. Postolovska. “Very often, they experience an increased level of anxiety. Our questions about their medical history cause individual associations, and memories with home. Some of them perceive it normally, but it is rather painful for those who have no place to return to."
Patients who need specialized help are referred to psychological teams. Sometimes, doctors themselves also require psychological support.
"Although we know how to cope with stressful situations, somehow we empathize and plunge into this state,” said Dr. Postolovska. “The concerns of many Ukrainians are similar, and we also share this pain. If necessary, we turn to the centre’s psychologist to be able to keep fighting on our front."
Despite the difficulties, the gynaecologist says that the work inspires her.
"Obstetrics and gynaecology is a spiritual field with many factors that help us to recover,” she said. “Cured women, pregnancy of those who had infertility, newborn children – all of this reminds us that life continues - even during war."
Thankful to support from Denmark, ECHO and CERF, UNFPA sexual and reproductive health mobile teams and clinics work in 21 regions of Ukraine to ensure effective medical assistance to women and girls in the most remote areas.


